
« Centre multidisciplinaire intégré, unique en Belgique et reconnu internationalement, l’Institut Jules Bordet est un hôpital entièrement consacré aux patients atteints de maladies cancéreuses. Depuis plus de 75 ans, nos équipes proposent aux patients des stratégies diagnostiques et thérapeutiques à la pointe du progrès pour prévenir, dépister et lutter activement contre tous les types de cancers. L’Institut Jules Bordet mène aussi d’importantes activités de recherche menant chaque année à des découvertes majeures et dispense un enseignement universitaire spécialisé de haut niveau »
Titre
Nos missions
Les soins cliniques
La spécificité de l’Institut Jules Bordet réside dans la réelle multidisciplinarité des approches de soins tant en ce qui concerne le diagnostic que le traitement et les soins de support. Tant pour assurer le diagnostic le plus précis possible que pour prendre les décisions quant aux meilleurs traitements, les médecins de plusieurs spécialités différentes (oncologues, chirurgiens, radiothérapeutes, etc), les paramédicaux, les infirmiers et les psychologues réfléchissent ensemble et se concertent. Ces stratégies thérapeutiques font appel aux techniques les plus modernes.

La recherche
Un aspect fondamental de l’Institut Jules Bordet est l’étroite intégration de la recherche à la pratique médicale quotidienne, permettant ainsi aux patients de participer à des études cliniques sur de toutes nouvelles modalités thérapeutiques et de bénéficier le plus rapidement possible des dernières découvertes faites dans les laboratoires de recherche. De nombreux programmes de recherche clinique sont menés en coopération avec d’autres centres du cancer et réseaux nationaux et internationaux.

L'enseignement
Sur le plan académique et dans le cadre des missions qui lui ont été confiées par l’Université Libre de Bruxelles, l’Institut Jules Bordet est réputé pour la qualité de l’enseignement qu'il prodigue tant aux médecins qu'aux autres catégories de professionnels de santé (infirmiers, paramédicaux, psychologues, technologues de laboratoire, etc). Chaque année, des dizaines d’étudiants en médecine et de médecins en cours de spécialisation viennent se former auprès de nos équipes médicales.

Titre
Hôpital Universitaire de Bruxelles (H.U.B)
L'Hôpital Universitaire de Bruxelles (H.U.B) est l’Hôpital Académique de l’Université Libre de Bruxelles (ULB) qui regroupe l’Institut Jules Bordet, l’Hôpital Erasme et l’Hôpital Universitaire des Enfants Reine Fabiola (HUDERF) depuis 2021. En tant que centre de référence de niveau international, implanté au cœur de la région bruxelloise, l’H.U.B propose des soins généraux, oncologiques et pédiatriques de grande qualité. Ces soins d’excellence, accessibles à toutes et tous, sont enrichis et nourris par une double démarche de recherche scientifique et d’enseignement pour les soignants de demain. En 2022, l’H.U.B se compose de plus de 6000 collaborateurs qui portent les valeurs suivantes : Intérêt du patient, Esprit d’équipe, Engagement, Solidarité, Diversité et Inclusion et Libre examen.

Titre
Travailler à l'Institut
Avec plus de 1000 collaborateurs, l’Institut Jules Bordet regroupe l’ensemble des disciplines médicales et paramédicales liées au traitement des différents types de cancers.
Notre objectif : offrir au patient un environnement de soins efficaces, agréable et à dimension humaine.
Pour atteindre cet objectif, le Département des Ressources Humaines joue un rôle clef dans l’organisation en soutenant l’ensemble des équipes multidisciplinaires.

Jules Bordet, pionnier dans la recherche contre le cancer
Depuis sa création, en 1939, l'Institut Jules Bordet s’est toujours inscrit en pionnier dans la lutte contre le cancer, cette maladie complexe aux mille visages. Face à ces pathologies, les destins des patients et des soignants font plus que se croiser ; ils se lient. Sans prétention d’exhaustivité, rappelons quelques dates clés de l’histoire de l’Institut Jules Bordet, fier de son passé et résolument tourné vers l’avenir.
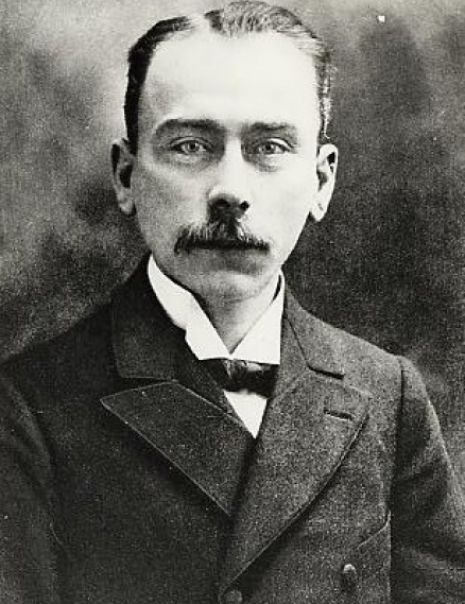
Jules Bordet
Docteur en médecine, spécialiste en bactériologie et en immunologie.
Prix Nobel de Physiologie et de Médecine en 1919.